RazorMetrics’ drug cost survey reveals consumers want their physician to take the lead on lowering their prescription costs.
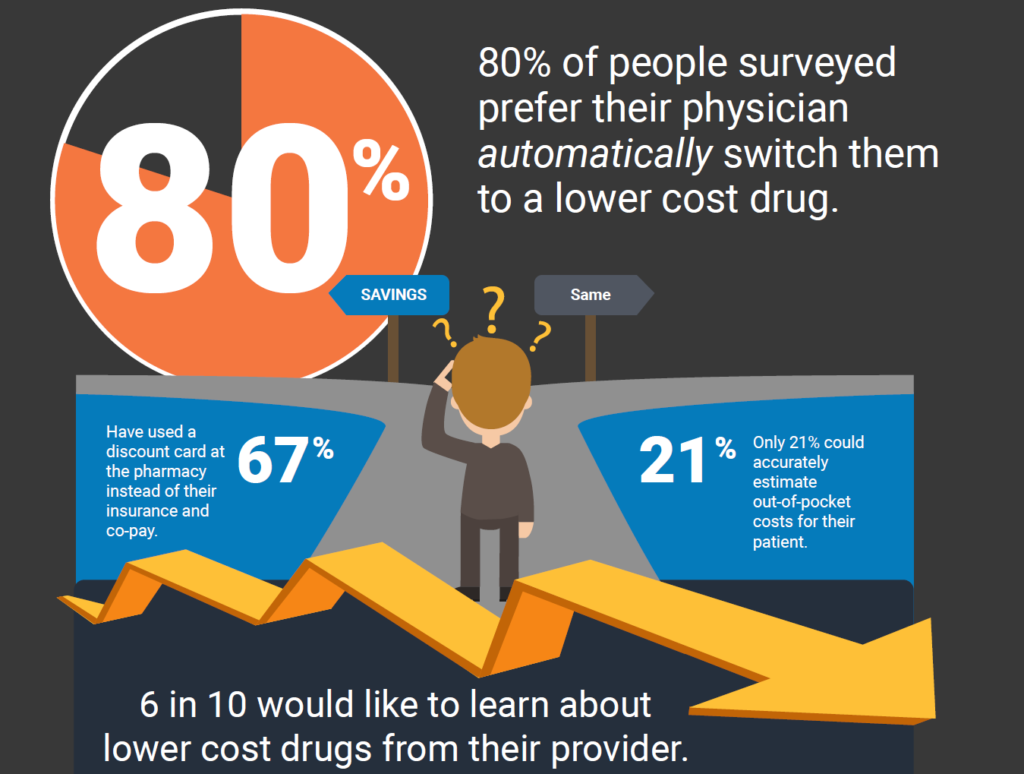
Austin, Texas (April 20, 2022) — RazorMetrics, an innovative healthcare technology company, recently conducted a consumer opinion survey asking about drug costs and found some surprising results. Despite the explosion in consumer-oriented drug savings options – mail-order pharmacy, discount cards, etc. – healthcare consumers want their physician to take the lead on lowering drug costs. The survey found that 80% of respondents would prefer their physician be the one to choose a lower-cost drug for their prescription and do so automatically.
Sticker shock at the pharmacy is a lose-lose situation for everyone. Each January, drug costs go up and people with monthly prescriptions see their pharmacy bills increase significantly. In January 2022, companies raised costs on 810 drugs by an average increase of 5.1%, which was greater than the rate of inflation last year (4.7%).
Over the past several years, Congress has hosted several hearings on the issue of escalating drug prices. However, there has been no significant legislation to fix the problem despite devastating stories about patients living in pain because they cannot afford their medication.
Jack Resneck Jr., MD, chair of the AMA Board of Trustees told members of Congress during a House Energy and Commerce Committee Health Subcommittee hearing, “Physicians see every day that costs are a major obstacle to our patients getting the right medication at the right time.” He continued, “I currently have a patient unable to afford the Enbrel or Humira that would alleviate his psoriasis and painful psoriatic arthritis—the average wholesale prices for a year of these drugs, both out for more than 15 years—has quadrupled to around $80,000 per year, and his PPO copay is 40% until he reaches his deductible. So, he stopped his treatment.”
This story is not unique. The high cost of prescriptions is often the cause for skipped doses, pill splitting, or discontinuing treatment altogether. Inconsistencies in refill cadence and medication adherence interrupt treatment resulting in a decrease in health status and an increase in emergency room visits. The website Patients for Affordable Drugs dedicates a page to patient horror stories about lifesaving yet unaffordable and out-of-reach medication dilemmas.
RazorMetrics’ drug cost survey uncovered a similar finding. When asked, “if a prescription is too expensive what do you do?” 9.3% of survey respondents said they “Forget about it and go home.” Other responses included “Pay for it anyway” (22.3%), “Ask the pharmacist about a discount” (35.3%), “Call my doctor” (21.7%), and “Call my insurance company” (11.3%). To patients, physicians, and pharmacists none of these options is satisfactory. Each of these choices represents wasted time and effort and an increase in health complications – both of which could be avoided.
When asked “if a prescription is too expensive what do you do?”
- 9.3% said, “Forget about it and go home.”
- 22.3% said, “Pay for it anyway.”
- 35.3% said, “Ask the pharmacist about a discount.”
- 21.7% said, “Call my doctor.”
- 11.3% said “Call my insurance.”
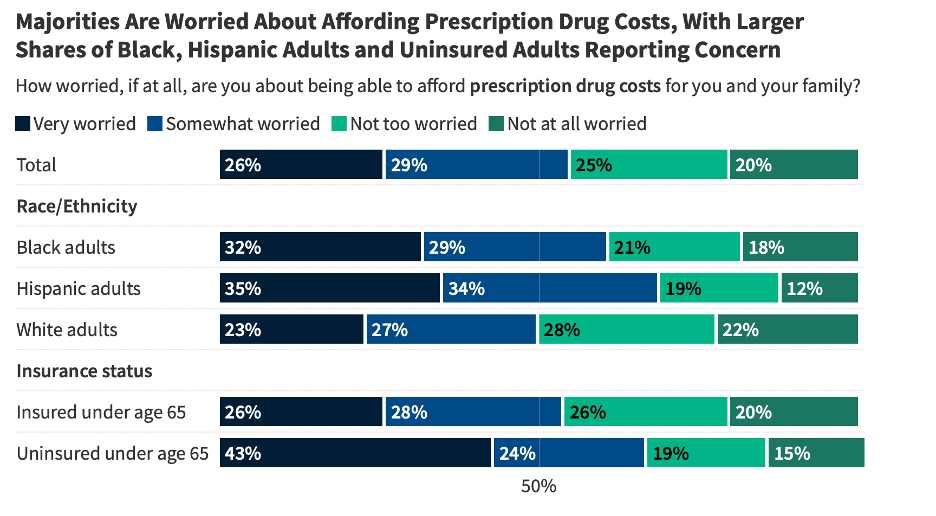
Physicians are making a strong effort to address the high cost of prescriptions. Seventy-two percent of survey respondents said that their physician talks to them about drug prices and generics. The problem is that physicians cannot estimate the cost of medication due to a lack of data intelligence. When writing a script, physicians don’t know what the cost will be to the patient. This finding is backed up by another study published in Jama Network Open, “Accuracy of Physician Estimates of Out-of-Pocket Costs for Medication Filling.” In the study, Dr. Sloan found that when physicians were given all the necessary information about a drug’s price and the patient’s insurance plan, only 21% could accurately estimate out-of-pocket costs for their patient. The layers of costs between the co-pay, formulary, rebates, coinsurance, deductibles, and other mechanisms were too complicated and opaque.
According to the study authors, “one-third of US residents have trouble paying their medical bills. They often turn to their physicians for help navigating health costs and insurance coverage.” This sets the physician up for failure even when given the information, it is too complicated to accurately estimate costs in a way that is helpful to their patients.
“As a cardiologist with an active practice, I can attest to the frustration doctors feel when we get a call from a patient at the pharmacy. We try another medication hoping that it will be covered by the patient’s health plan. The system is built on a trial by error model,” said Dr. Siva Mohan, MD, and co-founder of RazorMetrics. “It’s inefficient and deeply frustrating for everyone involved.”
Most solutions target consumers directly, putting the burden on patients to find the most affordable medication option. Many consumers are not adopting the required technologies that enable consumer-first decisioning. For example, while consumers could save hundreds or even thousands of dollars a year by switching to a discount mail order pharmacy, only 47% of respondents have tried it. And though insurers can choose to automatically move members to a mail-order model as a strategy to lower drug costs, only 5% of those surveyed by RazorMetrics have done so.
The survey results on mail-order are consistent with other national data. In 2020, a CoverMyMeds survey found that about 50% of patients surveyed received their prescriptions through mail order or pharmacy delivery (12% mail order, 25% combination of mail order and in-person, 13% home delivery by local pharmacy). This was a dramatic change over 2019 when 88% of patients got their prescriptions at an in-person, retail pharmacy. More pharmacies are getting into the delivery game but not all mail order is less expensive.
Among those surveyed by RazorMetrics, 69% said they would be open to trying mail order pharmacy. Dr. Mohan said, “The trick is making the change to mail order easy and ensuring the pharmacy is demonstrably less expensive. RazorMetrics’ has the ability to communicate this information to the physician, who then can feel comfortable making the recommendation to the patient.”
Discount cards are making headway tackling drug costs in the consumer market. Sixty-seven percent of RazorMetrics’ survey respondents reported using a discount card at least once. Discount cards could help the 49% of Americans that use at least one prescription medication every month. The most popular company among survey respondents was GoodRx by a large margin (56.5%). Pharmacy Supplied Discount (16.5%) and Amazon Prime Rx (19%) were the next popular. OptumRx Perks (2%), SingleCare (5.5%), and ScriptSave Well Rx (0.5%) were less represented among the survey pool.
The benefit of a discount card is that it allows people to pay cash for medications and forgo the co-pay and insurance route. This is a win for the patient because they pay less out of pocket as well as a win for the health insurance company since the medication goes completely off their books.
Discount cards are beginning to make a dent but there is still a long way to go. GoodRx reports that they have saved $35 billion and helped more than 18 million people afford a prescription since 2011. Since the US spends about $348 billion per year on prescriptions, there is still a lot of opportunity to do more.
It’s clear most consumers want to save money on prescriptions, but rather than chase down lower drug options themselves, they would prefer that their physician help them navigate the process. A full 88% of RazorMetrics’ survey respondents said they would be more satisfied with their healthcare provider if they talked to them about drug prices. Two-thirds of respondents reported that they would have a more favorable opinion of their healthcare provider if they changed their prescription to a lower-cost option. Put simply, patients want their physician to lead in getting affordable prescriptions.
Download the infographic here.
About RazorMetrics
RazorMetrics is a healthcare technology company whose SaaS-based platform uses AI and ML to lower drug spend for health plans, self-insured employers, and consumers. RazorMetrics unique, physician-first approach process that is simple, and requires no extra clicks in the EHR and no external programs or apps to access. Switches are straightforward, easy to make, and the entire process stays within the normal clinical workflow. The platform is complementary to existing pharmacy initiatives and works with PBMs and other drug cost savings solutions to optimize results. RazorMetrics is fully scalable and customizable to each client’s unique variables and formularies. For more information, visit razormetrics.com.
Media Contact:
Casey DeMoss, RazorMetrics
504-982-0468