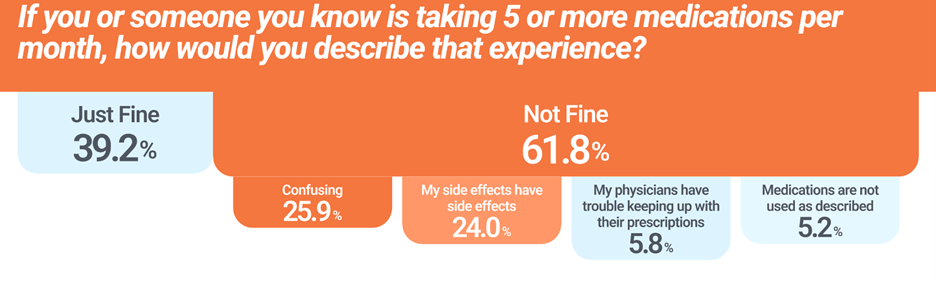
Polypharmacy, defined as taking five or more medications a month, may be appropriate, but it is not without risks. RazorMetrics’ report, the State of Drug Access, 2024 found that almost 62% of consumers had trouble with polypharmacy stating side effects, confusion, complicated regimens, and other problems. Problematic polypharmacy needs to be addressed when the medications are prescribed inappropriately, fail to provide the intended benefits, or cause harm. Being over-medicated predominantly affects older adults but is also significant for children and younger adults with chronic conditions and those with mental health problems.
Drawbacks of Polypharmacy:
- Non-Adherence. Medication overload can cause patients confusion. Many pills look similar, some medication is taken with food, prescription refills are on different schedules, and some meds are taken at night while others are taken in the morning. The confusion reduces compliance and treatment effectiveness.
- Increased Risk of Adverse Drug Events. More medications mean there is a higher potential for adverse interactions leading to harmful reactions, side effects, altered metabolism, and toxicity.
- Prescribing cascades. When the side effects of one drug are treated by another prescription, a vicious, self-perpetuating cycle results.
- Increased Hospitalization Risk. The increased risk of adverse drug events from polypharmacy leads to preventable hospitalizations and higher healthcare costs.
Counteracting Polypharmacy
Deprescribing is the process of reducing the dosage or stopping medications altogether that are no longer beneficial or may be causing harm. The physician typically takes this approach after a full medication review to reduce the medication burden and improve patient outcomes. Research has shown that reducing medications can reduce the risk of falls, improve cognitive function, lower hospitalization rates, and improve longevity for older adults.
Deprescribing Challenges
Physicians may be hesitant to initiate deprescribing when a medication is from a different prescriber. The full medication list may not be visible to every physician. For example, specialists may be in a different health system with an EHR that does not connect to the patient’s primary physician. Physicians are more likely to address side effect complaints with a new prescription rather than taking a prescription away. Also, organizational challenges and time constraints within healthcare systems limit the opportunity for thorough patient engagement.
According to Dr. Harmanleen Singh’s research and RazorMetrics, best practices for deprescribing are the following:
- Engage with the Patient: Gather information about the patient’s medications, their benefits, side effects, and adherence levels.
- Identify Inappropriate Medications: Assess each medication’s current clinical benefit and consider removing those that no longer provide a significant advantage or are potentially harmful.
- Shared Decision-Making: Collaborate with the patient to make informed decisions about deprescribing. This includes planning and implementing a safe medication withdrawal strategy, often involving dose tapering and continuous monitoring.
- Make it Easy for Physicians: The average time for a clinic to track down the full medication list for a single patient is 10 minutes. HealthTech can cut that time to less than one minute.
Balancing the benefits with the risks of new prescriptions is crucial for patient health and managing healthcare costs. Achieving best prescription practices, HealthTech can fill the gap for physicians by providing full medication lists to each patient’s prescriber, regardless of network, and prompting a discussion around polypharmacy. Since physicians are the authorized prescribers, they must lead the process of medication review, deprescribing, and patient conversations to improve health outcomes and lower healthcare costs.
To research more on this topic, please see the following:
State of Drug Access, 2024 by RazorMetrics
Lecture by Dr. Harmanleen Singh, The harms of prescribing: Polypharmacy, Deprescribing, and conducting research at medical school. Singh’s research, particularly on statins, highlighted that patients were often more willing to consider deprescribing than doctors anticipated. Effective deprescribing requires a collaborative approach involving guidelines and frameworks from relevant healthcare authorities to support clinicians in overcoming uncertainties and facilitating patient engagement.
Seminar by Dr. Holly M. Holmes, Hope and Healing Center & Institute Seminar on Polypharmacy: What Is It, and How Do I Avoid It? The lecture covers the dangers of polypharmacy and defines medication overload, ways to address it, types of drugs to avoid, and how to have a conversation with a healthcare provider about polypharmacy risks.